When biosimilars crashed into AbbVie's Humira in 2023, the pricing impact was mostly negligible. Now, that's beginning to change, and the Inflation Reduction Act could exacerbate how biosimilars affect branded medications, potentially slashing billions from healthcare costs.
A new study from Harvard University researchers examined the likely impact of the IRA on biosimilar coverage in Medicare, predicting that 2025 will take coverage away from brand-name biologics in favor of cheaper versions. The findings come as other reports suggest biosimilars in the commercial market are finally finding their footing.
Biosimilar barriers
At the end of 2023, biosimilars still had a lackluster presence, including low sales numbers and negligible market share for the handful of biosimilar versions of AbbVie’s rheumatoid arthritis drug Humira. Notably, the U.S. Humira biosimilar market share only reached 4% as of February 2024, according to a report from Samsung Bioepis, the maker of one of those copycats. But after CVS Health made the decision to drop Humira from its formulary this year, biosimilar prescriptions are picking up, Axios reported.
The market penetration of biosimilars has been better in the commercial space than for Medicare and other government plans, said Luca Maini, one of the authors of the study and an assistant professor of health care policy at Harvard Medical School.
Why haven’t biosimilars taken off faster? According to Maini, the market is still young.
“Physicians, patients and PBMs, and all the stakeholders, need to be comfortable with the idea that biosimilars … are just as safe and effective as originator biologics.”

Luca Maini
Assistant professor of health care policy, Harvard Medical School
“[There’s] a little bit of a learning curve,” he said. “Physicians, patients and PBMs, and all the stakeholders, need to be comfortable with the idea that biosimilars … are just as safe and effective as originator biologics.”
Physicians have been reluctant to swap out brand-name biologics like Humira for biosimilars in the first few years of availability, according to a 2023 report by Spherix Global Insights.
Reimbursement design for Medicare has been another barrier that benefitted biologics over biosimilars until 2022 when one of the first IRA provisions kicked in. The Medicare Part B changes increased biosimilar reimbursement rates, encouraging more competition with originator biologics.
Biologics are generally more intensive for patients compared to small molecules, according to Maini, who said these drugs are likely administered in a physicians’ office or require training by a healthcare professional before they can be administered at home.
“It's a lot harder for a biosimilar to immediately grab a large share of the market upon approval,” Maini said.
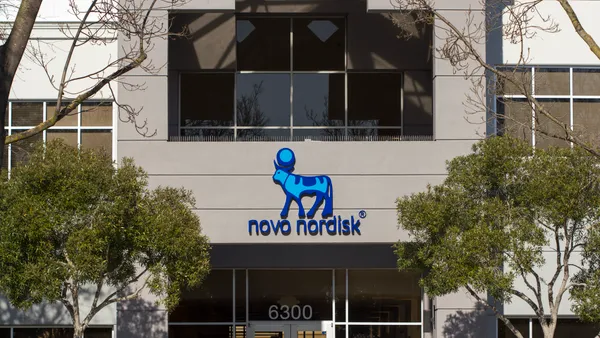
However, biosimilars are still making an impact, if AbbVie’s latest earnings are any indication. While still holding on to the majority of market share for Humira, AbbVie’s revenue declined at the start of the year, and that could lead the pharma to cut Humira’s prices down the road.
“If biosimilars come in and make no money, that's a problem because that is a signal to future biosimilar manufacturers that maybe it's not a good idea to launch the medicines,” Maini said. “If a biosimilar makes no money but ends up reducing the price of the originator by 40% or 50%, that is a success to some degree.”
The list price of Humira, for example, rose 141% between 2013 and 2020, according to the AJMC’s Center for Biosimilars. AbbVie enjoyed these “unsupported” price hikes despite a lack of new clinical data during the drug’s patent protection period, the Institute for Clinical and Economic Review noted.
Since the company’s patent cliff and biosimilars have become part of the equation — with nine biosimilar versions of Humira on the U.S. market by the end of 2023 — AbbVie has taken a hit, and the pharma slashed the price of Humira. The drug’s global revenues fell 36% during the first three months of 2024, according to recent earnings.
IRA impacts
The IRA's next biggest impact is expected to come from a change in the Medicare Part D benefit relating to catastrophic coverage through reduced federal subsidies.
“Medicare Part D tends to favor pricier reference biologic drugs over their generally cheaper biosimilar counterparts,” Maini and co-authors wrote in their analysis. “Two critical aspects of Medicare Part D benefit design likely contribute to this pattern: the federally mandated discounts for branded drugs for beneficiaries in the coverage gap and the federal subsidies given to plans during the catastrophic coverage phase.”
Currently, Medicare covers a significant portion of biologics once patients reach the catastrophic coverage phase, when out-of-pocket spending passes $8,000. At that point, Medicare covers 80% of the price of the drug, but the payment formula does not incentivize cheaper drugs.
“The patient is paying more money out of pocket and the plan is also paying more,” Maini said. “And that's because the government ends up picking up more of the tab for the expensive product than for the cheaper product.”
By closing the coverage gap in the catastrophic phase, the payment shift may realign coverage decisions in favor of biosimilars, the study predicted.
Legislation has already had an impact. Following the implementation of the Bipartisan Budget Act of 2018, biosimilar coverage increased 23% due to changes in formulary coverage for Medicare Part D, the study found. Discounts for biosimilars in the legislation led to more coverage for these drugs, and the researchers anticipate a similar shift with the IRA starting in 2025.
“We should already see an effect with the new year,” Maini said. “Firms need some time to adjust to new conditions, but I would expect to see an effect right away.”